Categories
Delusional Misidentification Disorders: Part 1 – Capgras Syndrome
Delusional Misidentification Disorders: Part 1 – Capgras Syndrome
Today’s discussion turns to a group of somewhat rare syndromes that are related to the concept of misidentification and are labeled together as Delusional Misidentification Syndromes (DMS). In these syndromes someone, or something, is incorrectly identified as a person, place or thing. Thoughts and attribution of thoughts are also misidentified, in many cases to the point of being delusional. Some of these syndromes are more often than not related to organic abnormalities of the brain, or they may be a combination of organic problems with psychological issues, or in rare instances, may be purely psychological. DMS is often associated with psychoses and has only rarely been reported in non-psychotic individuals. It is nevertheless fairly rare, occurring in about 4% of patients presenting with functional psychoses (Melca et al., 2012).
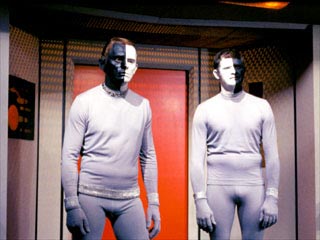
Capgras Syndrome is a misidentification syndrome where a person holds a delusion or belief that an acquaintance, typically a close family member, has been replaced by an identical looking imposter. This syndrome can be transient, developing very quickly after a brain injury, or can take a chronic form where the delusion is long standing. The syndrome is named after Joseph Capgras lived 1873-1950 French psychiatrist who first described the disorder in a 1923 paper and used the term ‘illusion of doubles’ to describe a case of woman who had various doubles that had taken the place of people she knew. For some people with Capgras syndrome, even inanimate objects such as chairs and animals can be imposters. Often patients are so disturbed with seeing their doubles that they remove all mirrors from house. In some cases, if the Capgras sufferer can be convinced that one person is not an imposter, they will develop a Capgras delusion with someone else. (Sinkman, 2008).
Many patients suffering from Capgras Syndrome have already been diagnosed with schizophrenia. However, Capgras Syndrome can also be co-morbid with other mental health problems including; Alzheimer’s Disease, Cotard’s Syndrome, epilepsy, Farh’s Disease, Fregoli Syndrome, Hashimoto’s Hypothyroidism, Incubus Syndrome, Neurodegenerative Disease, Diogenes Syndrome, Parkison’s Disease (Bourget & Whitehurst, 2004; Ceylan et al., 2010; Chiu, 2009; Donnelly et al., 2008; Fischer et al., 2009; Josephs, 2007; Mishra, Prakesh, Mishra, Praharaj, & Sinha, 2009; Pande, 1981; Rodríguez, Madoz-Gúrpide, & Ustárroz, 2011; Yalin, Taş, & Güvenir, 2008). Capras has also been associated with the administration of morphine and ketamine (Bekelman & Hallenbeck, 2006; Corlett, D’Souza, & Krystal, 2010).
Since the time Capgras Syndrome was first described (and even a bit before) a number of theoretical explanations have been put forth as to its origins. As might be expected many of these theories were psychoanalytically based in the early days. De Pauw (Sinkman, 2008) has written a comprehensive account of these early conceptualizations of Capgras. In this article de Pauw notes that many of the psychoanalytic explanations are mutually incompatible. These psychoanalytic theories include; defense against unconscious homosexuality, a regression to the early stage of primary narcissism, which some writers believe was due to anxiety, and a novel resolution to the Oedipal and especially the Electra complexes. Psychodynamic explanations seemed to make sense because the people being replaced by imposters were almost always close family members. However, on closer scrutiny of the literature this argument falls apart as other people or things are often found to also be imposters, from doctors and nurses to entire buildings and other inanimate objects. In general, according to de Pauw psychoanalytic explanations tend to be “generally post hoc and teleological in nature, postulating motives that are not introspectable and defense mechanisms that cannot be observed, measured, or refuted” (p. 158). He concludes that while the presence of brain injury also does not fully explain Capgras Syndrome it may be due to a breakdown in the manner in which sensory information is brought into the brain and the way it is stored (and presumably retrieved).
Another issue in the published case literature about Capgras Syndrome is the focus on the delusion of the imposter to the exclusion of other aspects of the syndrome. Closer scrutiny often demonstrates other DMS and psychotic/schizophrenic symptoms in Capgras cases. Many patients suffer from a sort of expanded Capgras Syndrome where there are many other delusions present. Some of these delusions may be somatic in nature with the patient experiencing bizarre changes to their bodies, with their seeming strange and alien. Even the patient’s sense of self is changed and subject to delusion. These symptoms are reminiscent of schizophrenia and it is no surprise that many cases of Capgras have a co-morbid diagnosis of schizophrenia, usually of the paranoid variety. Upon closer examination it can become difficult to make a differential diagnosis between Capgras and schizophrenia in many sufferers, and the Capgras symptoms may be another aspect of the schizophrenic illness. In fact, studies have shown that misidentification symptoms occur in a large number of cases of schizophrenia, maybe even as high as 40% (Sinkman, 2008).
Modern clinicians and researchers now believe that Capgras has an organic basis, which is specifically related to cerebral dysfunction. Neuroimaging studies have shown that lesions in the right hemisphere of the brain are common among Capgras sufferers. Some studies have demonstrated bilateral damage to the hemispheres in Capgras patients (Bourget & Whitehurst, 2004). In one small study 81% of Capgras sufferers also had neurodegenerative disease, usually involving the Lewy body. As would be expected, these Capgras sufferers were older than Capgras patients without neurodegenerative disease, who were more likely to also suffer from paranoid schizophrenia, schizoaffective disorder, methamphetamine abuse, or other cerebrovascular problems. 100% of patients with Capgras and Lewy body disease experienced visual hallucinations (Josephs, 2007).
Capgras patients are prone to acts of violence, especially against people they have misidentified (Bourget & Whitehurst, 2004). Given the relation of Capgras to paranoid schizophrenia this makes sense.
There is evidence to support the idea that an emotional processing module in the brain, especially as it related to feelings of familiarity and unfamiliarity, and its connection to facial recognition is flawed in Capgras sufferers (Pacherie, 2009). This flaw in emotional processing can be demonstrated via facial recognition tasks and eye movement patterns (Brighetti, Bonifacci, Borlimi, & Ottaviani, 2007; Grignon & Trottier, 2005; Walther et al., 2010). Similar differences in audio perceptions related to working memory have also been reported for Capgras sufferers (Papageorgiou, Lykouras, Ventouras, Uzunoglu, & Christodoulou, 2002). In one dramatic case a Capgras patient had sexual relations with his wife, thinking she was a ‘double’. He had no feelings of familiarity with his wife whatsoever and essentially felt as if he were having sex with a different woman; so much so that he even changed his sexual behavior. The authors (Thomas Antérion, Convers, Desmales, Borg, & Laurent, 2008) note that this may be the only known documentation of a patient who was able to make his wife into his mistress!
As might be expected the typical treatment for Capgras Syndrome is anti-psychotic medications. However, when anti-psychotic medication is only partially or not effective the use of electroconvulsive therapy has been shown to be helpful. This is especially the case when Capras is co-morbid with Parkinson’s Disease (Chiu, 2009).
Fregoli Delusion
References:
Bekelman, D. B., & Hallenbeck, J. (2006). Capgras Syndrome Associated with Morphine Treatment. Journal of Palliative Medicine, 9(3), 810–813. doi:10.1089/jpm.2006.9.810
Bourget, D., & Whitehurst, L. (2004). Capgras Syndrome: A Review of the Neurophysiological Correlates and Presenting Clinical Features in Cases Involving Physical Violence. The Canadian Journal of Psychiatry / La Revue canadienne de psychiatrie, 49(11), 719–725.
Brighetti, G., Bonifacci, P., Borlimi, R., & Ottaviani, C. (2007). “Far from the heart far from the eye”: Evidence from the Capgras delusion. Cognitive Neuropsychiatry, 12(3), 189–197. doi:10.1080/13546800600892183
Ceylan, M. F., Bulut, M., Virit, O., Selek, S., Bülbül, F., & Savaş, H. A. (2010). Hashimato tiroiditi olan erişkin bipolar bozukluk hastasinda capgras ve fregoli sendromu birlikteliği. Yeni Symposium: psikiyatri, nöroloji ve davraniş bilimleri dergisi, 48(1), 69–71.
Chiu, N.-M. (2009). Repeated electroconvulsive therapy for a patient with Capgras syndrome and Parkinsonism. Progress in Neuro-Psychopharmacology & Biological Psychiatry, 33(6), 1084–1085. doi:10.1016/j.pnpbp.2009.06.003
Corlett, P. R., D’Souza, D. C., & Krystal, J. H. (2010). Capgras syndrome induced by ketamine in a healthy subject. Biological Psychiatry, 68(1), e1–e2. doi:10.1016/j.biopsych.2010.02.015
de Pauw, K. W. (1994). Psychodynamic approaches to the Capgras delusion: A critical historical review. Psychopathology, 27(3-5), 154–160.
Donnelly, R., Bolouri, M. S., Prashad, S. J., Coverdale, J. H., Hays, J. R., & Kahn, D. A. (2008). Comorbid Diogenes and Capgras syndromes. Journal of Psychiatric Practice, 14(5), 312–317. doi:10.1097/01.pra.0000336759.50060.5c
Fischer, C., Keeler, A., Fornazzari, L., Ringer, L., Hansen, T., & Schweizer, T. A. (2009). A rare variant of Capgras syndrome in Alzheimer’s disease. The Canadian Journal of Neurological Sciences/ Le Journal Canadien Des Sciences Neurologiques, 36(4), 509–511.
Grignon, S., & Trottier, M. (2005). Capgras Syndrome in the Modern Era: Self Misidentification on an ID Picture. The Canadian Journal of Psychiatry / La Revue canadienne de psychiatrie, 50(1), 74–75.
Josephs, K. A. (2007). Capgras syndrome and its relationship to neurodegenerative disease. Archives of Neurology, 64(12), 1762–1766.
Melca, I., Rodrigues, C., Serra-Pinheiro, M., Pantelis, C., Velakoulis, D., Mendlowicz, M., & Fontenelle, L. (2012). Delusional Misidentification Syndromes in Obsessive–Compulsive Disorder. Psychiatric Quarterly, 1–7. doi:10.1007/s11126-012-9237-z
Mishra, B. R., Prakesh, R., Mishra, B. N., Praharaj, S. K., & Sinha, V. K. (2009). Capgras syndrome associated with Fahr’s disease. The Journal of Neuropsychiatry and Clinical Neurosciences, 21(3), 354–355. doi:10.1176/appi.neuropsych.21.3.354
Pacherie, E. (2009). Perception, emotions, and delusions: The case of the Capgras delusion. In T.
Bayne & J. Fernández (Eds.), Delusion and self-deception: Affective and motivational influences on belief formation., Macquarie monographs in cognitive science (pp. 107–125). New York, NY US: Psychology Press.
Pande, A. C. (1981). Co-existence of incubus and Capgras syndromes. The British Journal of Psychiatry, 139, 469–470. doi:10.1192/bjp.139.5.469
Papageorgiou, C., Lykouras, L., Ventouras, E., Uzunoglu, N., & Christodoulou, G. N. (2002). Abnormal P300 in a case of delusional misidentification with coinciding Capgras and Fŕegoli symptoms. Progress in Neuro-Psychopharmacology & Biological Psychiatry, 26(4), 805–810. doi:10.1016/S0278-5846(01)00293-7
Rodríguez, R. H., Madoz-Gúrpide, A., & Ustárroz, J. T. (2011). Propuesta de una batería neuropsicológica para la exploración del síndrome de Capgras. Revista Española de Geriatría y Gerontología, 46(5), 275–280. doi:10.1016/j.regg.2011.06.001
Sinkman, A. (2008). The syndrome of Capgras. Psychiatry: Interpersonal and Biological Processes, 71(4), 371–378. doi:10.1521/psyc.2008.71.4.371
Thomas Antérion, C., Convers, P., Desmales, S., Borg, C., & Laurent, B. (2008). An odd manifestation of the Capgras syndrome: Loss of familiarity even with the sexual partner. Neurophysiologie Clinique/Clinical Neurophysiology, 38(3), 177–182. doi:10.1016/j.neucli.2008.04.003
Walther, S., Federspiel, A., Horn, H., Wirth, M., Bianchi, P., Strik, W., & Müller, T. J. (2010). Performance during face processing differentiates schizophrenia patients with delusional misidentifications. Psychopathology, 43(2), 127–136. doi:10.1159/000277002
Yalin, Ş., Taş, F. V., & Güvenir, T. (2008). The coexistence of Capgras, Fregoli and Cotard’s syndromes in an adolescent case. Nöropsikiyatri Arşivi/Archives of Neuropsychiatry, 45(4), 149–151.




2 replies on “Delusional Misidentification Disorders: Part 1 – Capgras Syndrome”
This comment has been removed by the author.
LikeLike
Interesting article. Reminds me of a man I rented a room from a few years ago. For his privacy I'll give the man a fictitious name – Will.
I lived with Will for approximately 1.5 years. Will seemed to be a healthy, strong, and high functioning older man but on permanent disability. I never understood why he'd be on disability and also never felt it was my place to ask.
Will began exhibiting odd behavior and one of two things began happening. Either Will was going through an active phase or as I was finishing up an undergrad psychology degree I began hunting for psychosis. I believe the former is closer to the truth.
There is a science fiction that claims lizard people are snatching humans, killing them, and keeping their outer dermis to infiltrate society and hold high political, media, financial and other positions of power. There are several accounts of this and from what I understand became highly popular in the 80's and recently again in a TV show called “V” (good show). The trouble for Will is he strongly identified with this science fiction, believing many persons of power were actually lizard people. His sister in law was among them. As the winter season approached and his persecutory themes deepened, other people close to him turned out to be lizard people as well. He revealed to me the his neighbor and possibly even a former roommate were among THEM and THEY. This extended to his father and possibly his older brother. Although the father/brother never definitively became lizard-people that I'm aware of Will was always contemplating that possibility.
As I began suspecting I might want to begin searching Craigslist for new digs a new behavior began taking shape. Certain items, inanimate objects, were either being treated, healed or removed from the house by Will. These objects, according to Will, either had been removed from the house at 4AM (specifically) and tampered with, or had been spiritually altered on some other dimensional level that they were now different and evil. Trying to be sympathetic to my roommates distress I learned from Will that these objects most often had strong memories associated with his late mother. These objects were also highly prized by his lizard incognito sister in law.
I responded because of the paragraph in the article that mentions how the idea of Capgras breaks down when the delusions extend to non-family members or objects. Will, whom in retrospect may have been co-morbid with Capgras, felt non-familial persons and inanimate objects were doubled or altered. But as Will's active phase became more apparent closer family members turned out to be lizard people and the objects he felt were doubled or altered had strong emotional ties to his mother. The emotional attachments were very polarized. Either invoking fond memories or fearful ones.
LikeLike