You can read or download it here:
You can read or download it from here:

I was on Wendy Walsh’s radio show last Sunday discussing the las Vegas shooter:
 Personality Disorders – The Common Bizarre Behaviors Part IV: The Role of Culture
Personality Disorders – The Common Bizarre Behaviors Part IV: The Role of Culture
In reality it is often difficult for clinicians to make a differential diagnosis among personality disorders as they share many key features in common. Some of the traits that are common to all personality disorders include:
Difficulty abiding by societal rules and conventions
Lack of empathy
Lack of hallucinations and overt thought disorders (except during brief psychotic episodes)
Lack of individual accountability
Lack of insight into how objectionable their behavior is to others
Lack of perspective
Self-centeredness
Superficial understanding of themselves
Vulnerability to other mental problems
Diagnosis often becomes an impression of the predominant features of the disorders rather than excluding one set of diagnostic criterion for another. Clinicians may also make a diagnosis based on what they believe to be the less stigmatizing personality disorder label (Aviram, Brodsky, & Stanley, 2006; Markham, 2003). There are gender differences in the prevalence of types of personality disorders. Antisocial personality disorder is more common among males, while borderline, dependent, and hysterical personality disorders are more common among females. Labeling biases among health professionals may explain some of these gender differences (Ussher, 2013). There is some evidence that clinicians may diagnose people with personality disorders based on the role stereotype of their status group (Landrine, 1989). Age may also complicate the diagnosis of personality disorders as well as introduce bias (Magoteaux & Bonnivier, 2009). And lastly, it seems that personality disorders may manifest in different ways depending on the cultural context of the person manifesting the disorder.
This is important because personality disorders tend to resemble many of the culture-bound syndromes, disorders, and behaviors found in cultures from all around the world. For instance, the culture-bound syndrome taijin kyofusho (which literally means fear of interpersonal relations) typically found in Japan and other parts of Asia, shares many of the features of avoidant and dependent personality disorders. The phenomena of latah, found primarily in Southeast Asia, carries echoes of borderline and histrionic personality disorders, while people who suffer from amok may show symptoms of antisocial and narcissistic personality disorders. It is difficult to fail to see the relationship between obsessive-compulsive personality disorder and the salaryman culture in Japan, just as it is difficult not to notice the schizotypal thinking present in koro. While these are just a few examples from around the world, we can also find similarities with personality disorders in our own Western culture. For example it is hard to miss the flavor of narcissistic and borderline personality disorders among some of the people who practice vampirism. Likewise, we see characteristics of antisocial, narcissistic, paranoid, and schizotypal disorders in the phenomena of school shooters – perhaps a Western version of the Southeast Asian cultural disorder amok.
So how do we understand the influence of culture to personality disorders? One thing we can try to do is to understand the relative influence of cultural characteristics in the different personality disorders. Alarcon & Foulks have attempted this in their 1995 paper. They list the personality disorders in a rank from the most ‘biologically based’ to the most ‘psychosocialculturally based’. This kind of ranking may make it easier to understand the influence of culture on each type of personality disorder. Alarcon & Foulks (1995, p. 84) also list each personality disorder in this ranking scheme with the characteristics of each disorder:
Schizotypal (Eccentric): Individualism, hyperintellectualization, hyperstimulation leading to excessive fantasy, self-affirmation, insocialbility.
Paranoid (Suspicious): Individualism, distrustfulness, rigidity, sense of oppressiveness, anger, adversarialism / antagonism, distorted sociability.
Schizoid (Asocial): Individualism, indifference, distorted self-sufficiency, hypostimulation, limited sociability.
Antisocial (Aggressive): Individualism, antagonism, conflict-proness, rigidity, need to prove self, anger, demonstrativeness.
Borderline (Unstable): Ambiguity, unpredictability, inconsistency, need to prove self, distorted sociability.
Obsessive-Compulsive (Conforming): Self-doubts, uncertainty, inconsistency, rigidity, frugalism.
Avoidant (Withdrawn): Inconsistency, sense of personal inferiority, no risk-taking, limited sociability.
Dependent (Submissive): Opaqueness, distorted sociability, unconditional rule following, search for paternalism.
Narcissistic (Egotistic): Individualism / selfishness, self-affirmation, grandiosity, emptiness, hypersociobility.
Histrionic (Gregarious): Social, instability, overstimulation, self-affirmation, demonstrativeness, materialism.
And lastly Alarcon and Foulks include an 11th characterization which, is not strictly a personality disorder:
Passive-Aggressive (Negativistic): Inconsistency, conflict-proness, distorted sociability, punitiveness.
This is an interesting way to understand the different personality disorders as each set of traits in the above descriptions may reflect characteristics of a patient’s cultural group and
“it would be incumbent upon the clinician to sort them out…and assign to them a diagnostic, as well as a therapeutic value. An analysis of the “symptoms” present in the above sets, from the perspective provided by different ethnic and cultural groups…might prove helpful to the clinician in differentiating PDs from non-pathological, culturally determined behavior.” (Alarcon & Foulks, 1995, p.84-85).
And in fact, this kind of an approach (similarly proposed by Paniagua, 2000) can be helpful in examining the ‘pathology’ of all culturally-significant behaviors, not just those that resemble personality disorders.
The connection between various culture bound syndromes and personality disorders deserves further study. While not everything defined as a culture bound syndrome is related to personality disorders, the prevalence of similarities suggests more than a coincidental connection. Personality disorders are indeed a world-wide phenomena. Our lack of understanding the etiology of personality disorders and the difficulty in treating them, suggests that the study of these serious disorders should be a priority for clinical psychology research.
References
Alarcon, R. D . & Foulks, E. F. (1995). Personality Disorders and Culture: Contemporary Clinical Views (Part B). Cultural Diversity and Mental Health, 1(2), pp. 79-91.
Aviram, R. B., Brodsky, B. S., & Stanley, B. (2006). Borderline Personality Disorder, Stigma, and Treatment Implications. Harvard Review Of Psychiatry (Taylor & Francis Ltd),14(5), 249-256.
Landrine, H. (1989). The politics of personality disorder. Psychology Of Women Quarterly, 13(3), 325-339.
Magoteaux, A. L., & Bonnivier, j. F. (2009). Distinguishing between personality disorders, stereotypes, and eccentricities in older adults. Journal Of Psychosocial Nursing And Mental Health Services, 47(7), 19-24.
Markham, D. (2003). Attitudes towards patients with a diagnosis of ‘borderline personality disorder’: social rejection and dangerousness. Journal Of Mental Health, 12(6), 595-612.
Paniagua, F. A. (2000). Culture-bound syndromes, cultural variations, and psychopathology. In Handbook of Multicultural Mental Health. Cuéllar, I., & Paniagua, F. A. (Eds). pp. 139-169. San Diego, CA, US: Academic Press.
Ussher, J.M. (2013). Diagnosing difficult women and pathologising femininity: Gender bias in psychiatric nosology. Feminism & Psychology, 23(1), pp. 63-69.
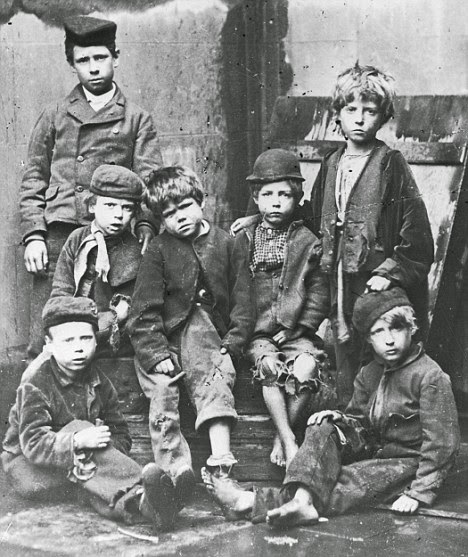
Origins of Personality Disorders
The cause of personality disorders is unknown. However, we do know that personality disorders are highly related to early child hood trauma, which can take the form of emotional, physical or sexual abuse, inconsistent parenting, and/or parental neglect (Dudeck, et. al., 2007; Griffin, 2004; Grover, et. al. 2007; Johnson, Sheahan, & Chard, 2003; Mclean & Gallop, 2003; Minzenberg, Poole, & Vinogradov, 2006; Modestin, 2006; Narisco, 2007; Seese, 1997; Semiz, Basoglu, Ebrinc, & Cetin, 2007) [1]. A study of personality disordered outpatients (who tend to have less severe symptoms) by Bierer, et. al. (2003) found only modest relationships between specific trauma dimensions and personality disorder diagnoses, though the general relationship between trauma and personality disorders was high. Sexual and physical abuse were specific predictors of paranoid and antisocial personality disorders, while emotional abuse predicted borderline personality disorder.
Interestingly enough, childhood sexual abuse does not seem to cause neuro-biological changes in people suffering from borderline personality disorder (Zweig-Frank, et. al., 2006), though numerous studies have now demonstrated neurological differences in personality disordered patients compared to normal controls (see section below).
Genetic and other environmental factors play important roles in the characteristics of some personality disorders. For instance, borderline personality disorder itself does not seem to be genetically determined and research has shown that most people with borderline personality disorder have suffered from abuse as children and that memories of this abuse are stable (Kremers, et. al. 2007). Nevertheless, some the key characteristics of this disorder, such as aggressiveness, impulsivity, suicidal tendencies, and emotional instability have been shown to be heritable (Coccaro, Bergman & McLean 1993; Bohman, et. al., 1984; Bouchard, 1994; Machizawa-Summers, 2007; Silverman, et. al., 1991; Togersen, et al, 1994; Torgersen, 2000).
A rule of thumb is ‘the worse the childhood the worse the personality disorder’, (Modestin, 2006; Vizard, Hickey, & McCrory, 2007) with more severe personality disorders being co-morbid with dissociative disorders (Sar, et. al., 2006). In another study childhood trauma and dissociative experience among patients with borderline personality disorder was related to emotional and physical abuse, and emotional neglect. Patients labeled as ‘high dissociators’ reported significantly greater levels of emotional/physical abuse, and emotional/physical neglect than low dissociators. Sexual abuse was not significantly related to dissociative experiences (Watson, et. al. 2006). In fact one study has demonstrated that people diagnosed with borderline personality disorder who do not report childhood sexual abuse are likely to achieve remission of the disorder in a relatively short amount of time Zanarini, et. al., 2006) [2].
At the more severe end of the personality disorder spectrum the patient may experience transient psychotic states. For patients at the severe end of this spectrum the distinction between a personality disorder and a psychosis can become a bit academic (Newton-Howes, et. al. 2008).
Neurobiology of Personality Disorders
There is quite a bit of promising research on personality disorders that examines the development of the brain. Traumatic events and/or inconsistent parenting are theorized to cause changes in the nerve pathways from the part of the brain where emotions are generated through the cerebral cortex where the emotions are regulated. As people with personality disorders have difficulty regulating emotions it is thought that areas of the brain related to emotional regulation may be dysfunctional. Using state of the art imaging technologies such as fMRI (functional magnetic resonance imaging) researchers have been able to show difference in brain function between people diagnosed with personality disorders and normal volunteers. This research not only gives hope for the development of new kinds of medication that may help personality disordered people better regulate their emotional states, but also may clarify the role of emotional regulation in human beings.
 One interesting line of research theorizes that neurological mechanisms underlying personality disorders may have evolved to help a person (really a child) adapt to a chaotic external environment. Lack of various types of empathy may have had survival value at different times in human evolution (Smith, 2006). In a chaotic, unstable, environment – say for instance a war zone – being in ‘fight or flight’ mode, labile emotional states and the ability to dissociate from one’s emotions, may have survival value (Austin, Riniolo, & Porges, 2007, Troisi, 2007). These kinds of chaotic and uncertain environments have characterized much of human and primate history. The deep and inherent nature of these mechanisms would also help explain why personality disorders are so very difficult to work with.
One interesting line of research theorizes that neurological mechanisms underlying personality disorders may have evolved to help a person (really a child) adapt to a chaotic external environment. Lack of various types of empathy may have had survival value at different times in human evolution (Smith, 2006). In a chaotic, unstable, environment – say for instance a war zone – being in ‘fight or flight’ mode, labile emotional states and the ability to dissociate from one’s emotions, may have survival value (Austin, Riniolo, & Porges, 2007, Troisi, 2007). These kinds of chaotic and uncertain environments have characterized much of human and primate history. The deep and inherent nature of these mechanisms would also help explain why personality disorders are so very difficult to work with.
The idea that personality disorders have at least a partially neurological genesis is not new. As early as 1946, Estabrooks theorized that strong emotional shocks, especially in childhood could ‘sensitize’ the brain causing personality disorders:
It matters little if the photographic plate of the brain, to use a very crude analogy, is exposed once in blinding light or 100 times in to the same object in dim light. The impression is, in the long run, just as definite and just as permanent (Estabrook, 1946, p. 204).
Modern views of personality disorders hypothesize that genetics, childhood trauma (and other environmental factors) are related to the characteristics of personality disorders such as emotional instability, impulsivity, aggression, and possibly cognitive and perceptual problems. These views have been arrived at not only through psychological studies, but increasingly through research on brain chemistry and structure (Goyer, Konicki, & Schultz, 1994).
One of the personality disorders most often studied is borderline personality disorder. Besides the obvious importance for understanding this destructive disorder the characteristics of the disorder lend themselves to better operational definition than the characteristics of other personality disorders. Typically, researchers have looked at impulsivity, aggression, (as well impulsive aggression), emotional instability, self-mutilation, and suicidal behaviors as indicators of borderline personality disorder. It may be that reduced serotonin transmission capacity in the brain may contributes to these negative traits among people suffering from borderline personality disorder. There is also research that suggests that the cholinergic system may be related to emotional instability, but that more work needs to be done to understand the physiology of this phenomenon. (Leyton, et. al. 2001; New & Siever, 2002; Zaboli, et. al., 2006).
A recent review of the research in this area conclude that impulsive aggression may involve deficits in central serotonin function as well as changes in the cingulate and medial and orbital prefrontal cortex. While these changes are hypothesized to be caused by early childhood trauma, this has not yet been definitively demonstrated. Borderline personality disorder has been shown to be biologically distinct from post-traumatic stress so the role of specific trauma is not yet known. Nevertheless, people with borderline personality disorder typically suffer from high rates of childhood abuse and neglect. It may be that the contribution of specific instances of trauma are less important than an overall long-term pattern of abuse in childhood. Studies of gene alterations that cause a reduction in serotonin have been shown to moderately affect impulsive and aggressive behavior and indicate that these aspects of borderline personality disorder may be inherited traits (Goodman, New & Seiver, 2004).
It may be true that people with the serotonin reducing genes may be more highly susceptible to traumatic childhood environment. A study by Reif, et. al. (2007) also found that genetic polymorphisms related to reduced serotonergic neurotransmission were related to violent behavior. The authors found that 45% of subjects carrying the low serotonin activity allele were prone to violent behavior compared to 30% with the normal serotonin activity allele. Subjects with the low serotonin activity allele who had experienced a highly adverse childhood environment were more likely to be violent later in life.
Brendel, Stern, & Silbersweig (2005) examined the interaction between negative emotion and lack of behavioral control. The authors report that abnormal frontolimbic circuitry is a likely suspect that explains the major clinical features of borderline personality disorder. These neuroimaging findings are integrated with developmental perspectives to explain the pathology associated with borderline personality syndrome, including the ways in which early childhood experience may interact with the developing brain.
The research on structural aspects of the brain also has demonstrated key differences in the brain of borderline personality sufferers when compared to normal people. One recent study by Silbersweig, et. al. (2007) examined impulse control in people with borderline personality disorder using functional magnetic resonance imaging technology. In order to assess impulse control the researchers asked subjects not to push a button when negative words were displayed. Normal subjects showed increased activity in the areas of the brain associated with emotional regulation and inhibition of limbic regions including the amygdala (orbitofrontal and cigulate cortices). These increases did not occur in people who suffered from borderline personality disorder. Also those with borderline personality disorder demonstrated increased activity in areas of the brain (dorsal anterior cingulated cortex) related to detection of conflict related to deciding on a response, suggesting that while they were unable to exercise impulse control, they had some awareness of the conflict inherent in the experimental situation. The research leads us to
…infer that when individuals with borderline personality disorder display decreased impulse control, this loss of impulse control may reflect a deficit in recruitment of brain mechanism of emotional regulation, and this process may be potentiated by context. Particularly stressful or negative contexts could lead to more impaired impulse control (Siegle, 2007, p. 1778).
Interestingly, the brain regions related to borderline personality disorder are also implicated in depression. Not surprisingly, borderline personality disorder and depression are often co-morbid. This suggests that treatment that works for some affective disorders may also help in borderline personality disorder. This may especially be true if contextual factors related to impulse control are included in the therapeutic regime (Brendel, Stern, & Silbersweig, 2005), and may explain why treatment such as Dialectic Behavior Therapy has proven successful with people suffering from borderline personality disorder (Siegle, 2007).
Next – Culture & Conclusions
References
Austin, M. A., Riniolo, T. C., & Porges, S. W. (2007). Borderline personality disorder and emotion regulation: Insights from the Polyvagal Theory. Brain and Cognition, 65(1), 69-76. doi: 10.1016/j.bandc.2006.05.007.
Bierer, L. M., Yehuda, R., Schmeidler, J., Mitropoulou, V., New, A. S., Silverman, J. M., & Siever, L. J. (2003). Abuse and Neglect in Childhood: Relationship to Personality Disorder Diagnoses. CNS Spectrums, 8(10), pp. 737-740.
Bohman, M., Cloniger, C.R., von Knorring, A., & Sigvardsson, S. (1984). An adoption study of somatoform disorders III: Cross-fostering analysis and genetic relationship to alcoholism and criminality. Archives of General Psychiatry, 41, pp. 872-878.
Bouchard, T.J. (1994). Genes, environment and personality. Science, 264(5166), 1700-1701.
Brendel, G. R., Stern, E., & Silbersweig, D. A. (2005). Defining the neurocircuitry of borderline personality disorder: Functional neuroimaging approaches. Development and Psychopathology, 17(4), pp. 1197-1206.
Coccaro, E.F., Bergman, C.S., & McLean, G.E. (1993). Heritability of irritable impulsiveness: A study of twins reared together and apart. Psychiatry Research, 48(3), p. 229-242.
Dudeck, M., Spitzer, C., Stopsack, M., Freyberger, H.J., & Barnow, S. (2007). Forensic inpatient male sexual offenders: The impact of personality disorder and childhood sexual abuse. Journal of Forensic Psychiatry & Psychology, 18(4), pp. 494-506.
Estabrooks, G.H. (1946). Brain sensitization in personality disorders. The Journal of General Psychology, 34, pp. 203-211.
Goodman, M., New, A., & Siever, L. (2004). Trauma, Genes, and the Neurobiology of Personality Disorders. In Yehuda, R., & McEwen, B. Biobehavioral stress response: Protective and damaging effects. New York, NY: New York Academy of Sciences, pp. 104-116.
Goyer, P. F., Konicki, P. E., & Schulz, S. C. (1994). Brain imaging in personality disorders In Silk, K. R. Biological and neurobehavioral studies of borderline personality disorder. Washington, DC: American Psychiatric Association, pp. 109-125.
Griffin, J. L. (2004). Structural equation modeling of Borderline Personality Disorder: Cognitive distortions, maladaptive schemas, psychological distress and insecure attachment as long-term sequelae of childhood sexual abuse. Dissertation Abstracts International: Section B: The Sciences and Engineering, 64(10-B), pp. 5216.
Grover, K.E., Carpenter, L.L., Price, L.H., Gagne, G.G., Mello, A.F., Mello, M.F., & Tyrka, A.R. (2007). The relationship between childhood abuse and adult personality disorder symptoms. Journal of Personality Disorders, 21(4), pp. 442-447.
Johnson, D. M., Sheahan, T. C., & Chard, K. M. (2003). Personality Disorders, Coping Strategies, and Posttraumatic Stress Disorder in Women with Histories of Childhood Sexual Abuse. Journal of Child Sexual Abuse, 12(2), pp. 19-39.
Kremers, I. P., Van Giezen, A. E., Van der Does, A. J. W., Van Dyck, R., & Spinhoven, P.H. (2007). Memory of childhood trauma before and after long-term psychological treatment of borderline personality disorder. Journal of Behavior Therapy and Experimental Psychiatry, 38(1), pp. 1-10.
Leyton, M. L., Okazawa, H. O., Diksic, M., Paris, J., Rosa, P., Mzengeza, S., Young, S. N., Blier, P., & Benkelfat, C. (2001). Brain regional [11C] methyl-L-tryptophan trapping in impulsive subjects with borderline personality disorder. American Journal of Pyshciatry, 158(5), 775-782.
Machizawa-Summers, S. (2007). Childhood trauma and parental bonding among Japanese female patients with borderline personality disorder. International Journal of Psychology, 42(4), Aug 2007. pp. 265-273.
McLean, L. M., Gallop, R. (2003). Implications of childhood sexual abuse for adult borderline personality disorder and complex posttraumatic stress disorder. American Journal of Psychiatry, 160(2), pp. 369-371.
Millon, T., Blaneyu. P. H., & Davis R. (eds.) (1999). Oxford Textbook of Psychopathology. New York: Oxford University Press. pp. 510.
Minzenberg, M. J. Poole, J. H., & Vinogradov, S. (2006). Adult social attachment disturbance is related to childhood maltreatment and current symptoms in borderline personality disorder. Journal of Nervous and Mental Disease, 194(5), pp. 341-348.
Modestin, J. (2006). Aetiology of personality disorders. Schweizer Archiv für Neurologie und Psychiatrie, 157(5), Jun 2006. pp. 221-226.
Narcisco, B. (2007). The relationships among trauma, self-concept, dissociation, Cluster B Personality Disorders and adult attachment style in incarcerated women. Dissertation Abstracts International: Section B: The Sciences and Engineering, 68(1-B), pp. 630.
Newton-Howes G, Tyrer P, North B, Yang M. (2008). The prevalence of personality disorder in schizophrenia and psychotic disorders: systematic review of rates and explanatory modelling. Preview Psychological Medicine, 38(8), pp. 1075-1082.
Reif, A., Rosler, M., Freitag, C. M., Schneider, M., Eujen, A. Kissing, C., Wenzler, D., Jacob, C. P., Retzt-Junginger, P., Thome. J., Lesch, K. P., & Retz. W. (2007). Nature and Nurture Predispose to Violent Behavior- Serotonergic Genes and Adverse Childhood Environment. Neuropsychopharmacology, 32, pp. 2375–2383.
Sar, V., Akyuz, G., Kugu, N., Ozturk, E., Ertem-Vehid, H. (2006). Axis I dissociative disorder comorbidity in borderline personality disorder and reports of childhood trauma. Journal of Clinical Psychiatry, 67(10), pp. 1583-1590.
Semiz, U., Basoglu, C., Cetin, M., Ebrinc, S., Uzun, O., & Ergun, B. (2008). Body dysmorphic disorder in patients with borderline personality disorder: prevalence, clinical characteristics, and role of childhood trauma. Acta Neuropsychiatrica, 20(1), pp. 33-40.
Siegle, G. J. (2007). Brain mechanisms of borderline personality disorder at the intersection of cognition, emotion, and the clinic. American Journal of Psychiatry, 164(12), pp. 1776-1779.
Silbersweig, D., Clarkin, J. F., Goldstein, M., Kernberg, O. F.,Tuescher, O., Levy, K. N., Brendel, G., Pan, H., Beutel, M., Pavony, M. T., Epstein, J., Lenzenweger, M. F., Thomas, K. M., Posner, M. I., & Stern, E. (2007). Failure of frontolimbic inhibitory function in the context of negative emotion in borderline personality disorder. American Journal of Psychiatry, 164(12), pp. 1832-1841.
Silverman, J.M., Pinkham, L., Horvath, T.B., Coccaro, E.F., Howard, K., Schear, S., Apter, S., Davidson, M., Mohs, R., & Siever, L.J. (1991). Affective and impulsive personality disorder traits in the relatives of patients with borderline personality disorder. American Journal of Psychiatry, 148(10), p. 1378-1385.
Smith, A. (2006). Cognitive empathy and emotional empathy in human behavior and evolution. Psychological Record, 56(1), 3-21.
Torgersen, S. (2000). Genetics of patients with borderline personality disorder. Psychiatric Clinics of North America, 23(1), p. 1-9.
Torgersen, S. (1984). Genetic and nosological aspects of schizotypal and borderline personality disorders: A twin study. Archives of General Psychiatry, 41(6), p. 546-554.
Troisi, A. (2007). The relevance of personality disorders for an evolutionary genetics of personality. European Journal of Personality, European personality reviews 2007., 21(5), 633-635.
Vizard, E., Hickey, N., & McCrory, E. (2007). Developmental trajectories associated with juvenile sexually abusive behaviour and emerging severe personality disorder in childhood: 3-year study. British Journal of Psychiatry: Special issue: Assessment, risk and outcome in severe personality disorder, 190(Suppl 49), pp. s27-s32.
Watson, S., Chilton, R., Fairchild, H., & Whewell, P. (2006). Association between childhood trauma and dissociation among patients with borderline personality disorder. Australian and New Zealand Journal of Psychiatry, 40(5), pp. 478-481.
Zaboli, G., Gizatullin, R., Nilsonne, A., Wilczek, A., Jonsson, E. G., Ahnemark, E., Asberg, M, & Leopardi, R., (2006). Tryptophan hydroxylase-1 gene variants associate with a group of suicidal borderline women. Neuropsychopharmacology, 31, pp. 1982-1990.
Zanarini, M. C. Frankenburg, F. R. Hennen, J., Reich, D. B., & Silk, K. R. (2006). Prediction of the 10-Year Course of Borderline Personality Disorder. American Journal of Psychiatry, 163(5), pp. 827-832.
Zweig-Frank, H., Paris, J., Kin, N. Y., Schwartz, G., Steiger, H., & Nair, N. V. (2006). Childhood sexual abuse in relation to neurobiological challenge tests in patients with borderline personality disorder and normal controls. Psychiatry Research, 141(3), 337-341. doi:10.1016/j.psychres.2005.02.009
—————
1. Literally hundreds of studies could have been listed here to support this statement. I have chosen to list only a few recent examples.
2. This also calls into question the reliability of the methods used for determining a diagnosis of borderline personality syndrome and would suggest that the predictors found in this study be used to rule out diagnosis of this disorder
—————
Co-Morbidity
Personality Disorders are among the least understood of the recognized psychological disorders. Unfortunately they are also the most common severe mental disorders. Their severity is compounded because personality disordered persons often have other medical or mental illnesses. More specifically, people suffering from personality disorders are more likely than the general population to also suffer from a history of alcohol and/or substance abuse (Bowden-Jones, et. al., 2004; Morganstern & Miller, 1997; Thuo, et. al. 2008; Volkan, 1994.), sexual dysfunction (Bogaerts, et. al., 2006; Maina, et. al. 2007; Neeleman, 2007; Hill, Habermann, Berner, & Briken, P. 2006), generalized anxiety disorder (Brooks, Baltazar, & Munjack, 1989; Hansen, et. al., 2007; Massion, et. al., 2002; Mavissakalian, et. al., 1995), bipolar disorder (George, et. al., 2003; Maina, Albert, Pessina, & Bogetto, 2007; Wilson, et. al., 2007), body-dysmorphic disorder (Semiz, et. al. 2008), obsessive-compulsive disorder (Hansen, et. al., 2007; Maina, Albert, Pessina, & Bogetto, 2007), depressive disorder (Wilson, et. al, 2007), post-partum depression (Akman, Uguz, & Kaya, 2007), eating disorders (Godt, 2002; Marañon, Echeburúa, & Grijalvo, 2004; Sansone, Levitt, & Sansone, 2005), post-traumatic stress disorder (Bollinger, et. al., 2000; Johnson, Sheahan, & Chard, 2003; Mclean & Gallop, 2003), self-mutilation (Andover, et. al., 2005; Dulit, et. al., 1994; Paris, 2005; Rollinick, 2001) and suicidal thoughts or acts (Pompili, Ruberto, Girardi, & Tatarelli, 2004).
Other maladaptive social consequences of personality disorders include decreased academic performance (King, 2000), domestic violence1 (Berger-Jackson, 2003), child molestation and sexual offense (Bogaerts, et. al., 2008; Dudeck, et. al., 2007), incarceration (Lindsay, et. al., 2006; Narisco, 2007), poor work habits and performance (Furnham, 2007; Kyrios, et. al. 2007; Lynch & Horton, 2004), and pathological gambling (Bagby, et. al. 2008; Samuels, et. al., 1994).
People diagnosed with one personality disorder often suffer from other personality disorders. In one study the majority of patients meeting criteria for a diagnosis of a personality disorders also were diagnosed with an additional personality disorder. The most prevalent personality disorders for the first diagnosis were avoidant, borderline, and obsessive-compulsive personality disorders. The authors suggest that patients suffering from personality disorders should be evaluated for additional personality disorders because their presence can influence the course and treatment (Zimmerman, Rothschild, & Chelminski, 2005).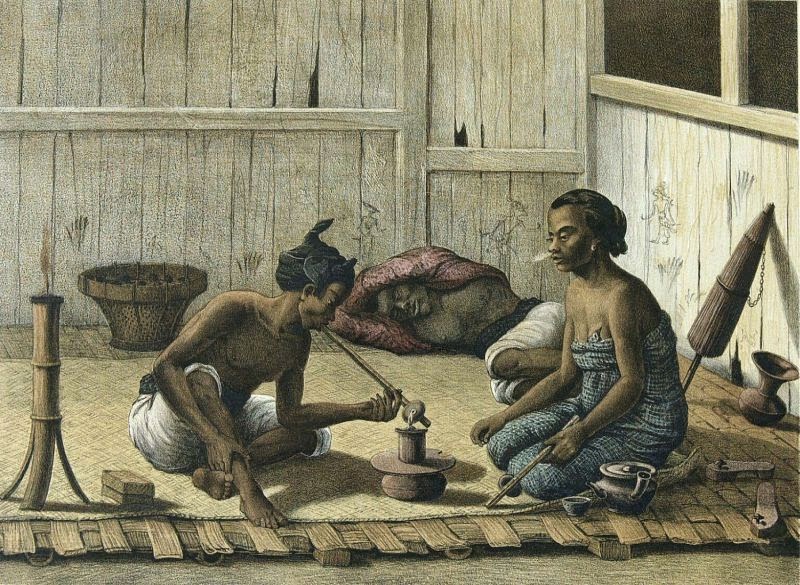
One of the most interesting things about personality disorders is that people around the one with disorder will be more distressed then the person manifesting the disorder. This distress may even be worse when the people close to the personality-disordered person are knowledgeable about the disorder (Hoffman, et. al., 2003; Scheirs & Bok, 2007). This fits in with many of our ideas about bizarre behaviors – they seem strange to us, but not the person exhibiting them.
Prevalence
Understanding personality disorders is important, as the prevalence of these disorders is quite high. For instance, a recent study found that 44% of volunteers for biomedical research studies suffered from a personality disorder (Bunce, et. al. 2005). Nevertheless the prevalence of personality disorders reported in the research is somewhat variable depending on the milieu and populations studied.
A good example of this variability can be seen in two studies conducted by the same first author. Moran et. al. (2000) examined the prevalence of personality disorder along with its relationship to sociodemographic status and common mental disorders in 300 primary care patients in the U.K.. They found a diagnosis of personality disorder in 24% of patients in the study. These personality-disordered patients were more likely to have past and present psychiatric problems, to be single, and to present to the surgery on an emergency basis when compared to non-personality disordered patients. Patients with cluster B personality disorders were particularly associated with psychiatric problems. The authors concluded that there is a high prevalence rate of personality disorders in the primary care setting and that this represents a significant source of burden.
However, two years later the same author reported relatively low rates for cluster B personality disorders in a similar population. Moran & Mann (2002) examined 303 primary care patients in southeast England for cluster B personality disorders. Using standardized assessment instruments they identified just 13 patients with personality disorders or a prevalence of 4% in their sample. The authors concluded that among primary care patients, cluster B personality disorders were uncommon.
Another study from a nearby geographical area, but situated in a community mental health clinic demonstrated much higher prevalence of personality disorders among their patients. This team of researchers from South London assessed personality disorders, as well as psychotic and affective disorders in their patient population. They found 52% of their patients met the criteria for one or more personality disorders, while 67 % of patients had a psychotic illness and 23 % had a diagnosis of a depressive disorder. Non-psychotic patients seen by nursing staff had extremely high rates of personality disorder, when compared to patients seen by psychiatrists and psychologists (Keown, Holloway, & Kuipers, 2002).
Using data from the 2001-2002 National Epidemiologic Survey on Alcohol and Related Conditions, Grant et. al. (2004) report that 14.79% of adults in the United States (approximately 30.8 million people) met the criterion for diagnosis of at least one personality disorder. The study did not include diagnoses for borderline, schizotypal and narcissistic personality disorders, which would have likely increased the incidence of personality order diagnoses. Of the personality disorders studied the most prevalent disorder was obsessive-compulsive personality disorder (7.9%), followed by paranoid personality disorder (4.4%), antisocial personality disorder (3.6%), schizoid personality disorder (3.1%), avoidant personality disorder (2.4%), histrionic personality disorder (1.8%), and dependent personality disorder (0.5%). Women had a significantly higher risk of avoidant, dependent, and paranoid personality disorders while men were at greater risk for antisocial personality disorder. No gender differences were seen for risk of obsessive-compulsive, schizoid, or histrionic personality disorders. Other risk factors for the personality disorders studied included being Native American, black, young adulthood, low socioeconomic status, and not having a significant other. Avoidant, dependent, schizoid, paranoid, and antisocial personality disorders were significant predictors of disability, while obsessive-compulsive personality disorder had an inconsistent relationship to disability. Individuals with histrionic personality disorder did not have any disability when compared with those without the disorder.
Bowden-Jones, et. al. (2004) found 37% of substance abusers and 53% of alcohol abusers in their sample also suffered from a personality disorder.
It is estimated that up to 50% of prisoners in the United States have antisocial personality disorder. This is likely due to the fact that behavioral characteristics associated with antisocial personality disorder, such as substance abuse, aggression, violence and vagrancy, are often related to criminal behavior. (Lindsay, et. al. 2006). In the U.K. the number of prisoners with antisocial personality disorder is 26%, less than the prevalence rates in the U.S., but still a substantial number (Hobson & Shine, 1998).
Clinical History & Treatment
Personality typically refers to those aspects of a person’s character that are not transient, i.e. ‘traits’, and opposed to ‘states’. According to Millon, Blaneyu, & Davis (1999):
Personality is seen today as a complex pattern of deeply imbedded psychological characteristics that are largely non-conscious and not easily altered, which express themselves automatically in almost every area of functioning. (pg. 510)
From this definition of personality the expectation is that traits associated with personality disorders would be stable over time. Recent studies support this idea (McGlashan, et. al. 2005). Therefore we can understand personality disorders (PDs) to be long-term, maladaptive patterns that pervade all aspects of a person’s life. These patterns include problems related to: perception (viewing and understanding the external world), ability to regulate emotions, high levels of anxiety, and poor impulse control. These patterns can lead to significant costs to both the person suffering from a personality disorder and the society he or she functions within. These costs, include lost productivity, increased interaction with law enforcement, imprisonment, a pattern of hospitalization, significant unhappiness, and suicide.
Personality disorders are notoriously difficult to treat. Long-term intensive psychotherapy has been shown to be effective for some personality-disordered patients (Bond, & Perry, 2004, 2006; Chatham, 1989). As Chatham puts it in regards to patients with borderline personality disorder;
I have observed that towards the end of the change process, patients often realize with surprise that early in psychotherapy certain things upset or traumatized them strongly enough to trigger various degrees of aberrant behavior. Basically, genuine improvement in borderline patients can begin only when primitive defenses and internalized pathological object relations have been uncovered and discarded. The patients must recognize that they can get on in the world without this pathology, because they now have moved forward in psychological development. But to get to this point sometimes requires a very long period of intensive psychotherapy (1989, p. 420).
According to Kernberg (1985), for this long-term intensive psychotherapy to be effective for people suffering from borderline personality disorders (or low ego strength – a defining characteristic of most personality disorders) the psychotherapy needs to be conducted by a skilled therapist who is in control of his or her own hostility and is not narcissistic. Therefore, while long-term psychotherapy for personality disorders is recommended there are may barriers to this type of treatment. Even if patients could afford and tolerate or afford this kind of treatment, finding the right therapist is crucial for a positive treatment prognosis. Short-term and supportive psychotherapy doesn’t seem to work as well as long-term intensive psychotherapy (Hoglend, 1993; Kernberg, 1985). Caligor, Kernberg, & Clarkin (2007) report on a transference-based object relations psychotherapy specifically designed for the treatment of personality disorders that appears to be effective.
Newer kinds of therapeutic techniques such as Cognitive-Behavior therapy and Dialectic Behavior Therapy (DBT) that was specifically designed to treat personality disorders show promise in effectively treating personality disorders2 (Davidson, et. al., 2007; Fruzzetti, 2002; Linehan, 1993; Linehan, et. al., 2007; Lynch, et. al., 2007; Salsman & Linehan, 2006; Sperry, 2006). Some question the long-term efficacy of these treatments, which seem to be measuring rather simple outcomes when compared to long-term psychodynamic treatment (Kernberg, 1985). Indeed, some research suggests that Cognitive-Behavior therapy works less well for personality disorders than for other types of mental problems (Luk, et. al., 1991). Another study indicates that the psychodynamic approaches may yield better long-term therapeutic results than Cognitive-Behavioral therapy with personality disordered patients (Leichsenring & Leibing, 2003). Nevertheless, Cognitive-Behavior therapy and Dialectic Behavior Therapy have shown efficacy in reducing acting out behaviors such as suicide attempts while being accessible (Davidson, et. al., 2006; Linehan, et. al., 2007). In fact, in one study the four major approaches to treating borderline personality disorders were all found to be successful in reducing behavioral acting out and affective instability, while not eliminating the underlying personality disorder (Lopez, et. al., 2007).
One of the dirty secrets of the psychotherapy profession is that many if not most therapists either consciously or unconsciously screen out patients with personality disorders (Hartman, 1999), or take on a ‘removed’ scientific attitude towards them (Davidtz, 2008). A UK study found that registered mental health nurses perceived patients with a diagnosis of borderline personality disorder more negatively than patients with a diagnosis of schizophrenia. Patients diagnosed with borderline personality disorder were perceived as more dangerous and were subject to more social rejection than those with a diagnosis of schizophrenia (Markham, 2003). Rothschild and Rand (2006) make the case that psychotherapists take on the emotional states of their patients through unconscious mirroring. This can cause vicarious trauma for psychotherapists, especially when they are unaware of their autonomic arousal. Since personality disordered patients have much more unstable emotional states it stands to reason that the psychotherapist will take on a much greater burden and a higher level of vicarious trauma when working with this patient population. As Fonagy says:
Why are these patients designated as difficult? Part of the difficulty undoubtedly arises out of the obligation we quickly feel as clinicians to enact that which is projected onto us. We are forced to be as our patients wish us to be, because we sense that without this, prolonged contact with us might be intolerable. They behave “unreasonably” toward us to elicit the reaction that they require, one which confirms for them that they have successfully externalized the alien part of the self. Because we try not to react in these directions in response to mild provocation, we unwittingly force our patients to become “more difficult.” They get under our skin and eventually discover what will make us react with anger, or what will cause us to neglect them, reject them, or feel excited by them, in all instances forgoing our therapeutic identity. (Fonagy, 1998, p. 1)
Indeed, we find that psychotherapists report personality-disordered patients as their most difficult (Davidtz, 2008). This is not only true in individual therapy but for group therapy as well (Liebenberg, 1990; Roth, Stone, & Kibel, 1990). Psychotherapists quickly learn that the amount of progress these patients make in therapy is disproportional to the amount of distress they inflict on the therapist. This sentiment has been born out on research studies that have shown that patients with personality disorders may have a propensity to engage in litigation with their therapist (Gutheil, 2005; Gutheil & Alexander, 1992), or their workplace (McDonald, 2002). This makes sense when examining the relationship between personality disorder-related phenomena such as suicide attempts and memories of child abuse which produce a good deal of the litigation directed towards mental health professionals (Gutheil, 2004). In the defense of psychotherapists, many are not trained to treat people with personality disorders, or only offer therapies that clearly do not work with these kinds of patients. In this way the screening of personality-disordered patients is justified as being better for both the therapist and the patient.
There are currently no drugs that directly treat personality disorders. Instead a number of different kinds of drugs are used to treat the symptoms associated with the personality disorder (Quante, et. al., 2008).
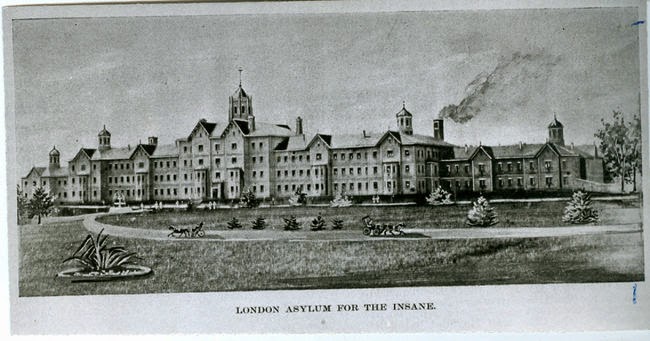
 The onset of personality disorders is usually in adolescents or early adulthood. However, a careful observer may be able to identify children who are likely to express these disorders later on. People who suffer from personality disorders, particularly Hysteric, Borderline, or Paranoid, end up with a greater chance of being hospitalized throughout their lives. This is due to a good deal of a suicidal behaviors, depression, alcohol/drug abuse, obsessive compulsive behaviors, eating disorders, domestic violence and other types of drama which are co-morbid with these personality disorders.
The onset of personality disorders is usually in adolescents or early adulthood. However, a careful observer may be able to identify children who are likely to express these disorders later on. People who suffer from personality disorders, particularly Hysteric, Borderline, or Paranoid, end up with a greater chance of being hospitalized throughout their lives. This is due to a good deal of a suicidal behaviors, depression, alcohol/drug abuse, obsessive compulsive behaviors, eating disorders, domestic violence and other types of drama which are co-morbid with these personality disorders.
Next – Origins & Neurobiology of Personality Disorders
References
Akman, C., Uguz, F., & Kaya, N. (2007). Postpartum-onset major depression is associated with personality disorders. Comprehensive Psychiatry, 48(4), pp. 343-347.
Andover, M. S., Pepper, C. M., Ryabchenko, K. A., Orrico, E. G., & Gibb, B. E. (2005). Self-mutilation and symptoms of depression, anxiety, and borderline personality disorder. Suicide and Life-Threatening Behavior, 35(5), pp. 581-591.
Bagby, R. M., Vachon, DD., Bulmash, E., & Quilty, L. C. (2008). Personality disorders and pathological gambling: a review and re-examination of prevalence rates. Journal of Personality Disorders, 22(2), pp. 191-207.
Berger-Jackson, L. (2003). Domestic violence link with personality disorders. Dissertation Abstracts International: Section B: The Sciences and Engineering, 63(10-B), pp. 4952.
Bogaerts, S., Vanheule, S., Leeuw, F., & Desmet, M. (2006). Recalled parental bonding and personality disorders in a sample of exhibitionists: A comparative study. Journal of Forensic Psychiatry & Psychology, 17(4), pp. 636-646.
Bogaerts, S., Daalder, A., Vanheule, S., Desmet, M., & Leeuw, F. (2008). Personality disorders in a sample of paraphilic and nonparaphilic child molesters: A comparative study. International Journal of Offender Therapy and Comparative Criminology, 52(1), pp. 21-30.
Bollinger, A. R., Riggs, D. S., Blake, D. D., & Ruzek, J. I. (2000). Prevalence of Personality Disorders Among Combat Veterans with Posttraumatic Stress Disorder. Journal of Traumatic Stress, 13(2), p. 255.
Bond, M., & Perry, J.C. (2004). Long-term changes in defense styles with psychodynamic psychotherapy for depressive, anxiety, and personality disorders. American Journal of Psychiatry, 161(9), pp. 1665-1671.
Bond, M., & Perry, J.C. (2006). Psychotropic medication use, personality disorder and improvement in long-term dynamic psychotherapy. Journal of Nervous and Mental Disease, 194(1), pp. 21-26.
Bowden-Jones, O., Iqbal, M. Z., Tyrer, P., Seivewright, N., Cooper, S., Judd, A., & Weaver, T. (2004). Prevalence of personality disorder in alcohol and drug services and associated comorbidity. Addiction, 99(10), pp. 1306-1314.
Brooks, R. B., Baltazar, P. L., & Munjack, D. J. (1989). Co-occurrence of personality disorders with panic disorder, social phobia, and generalized anxiety disorder: A review of the literature. Journal of Anxiety Disorders, 3(4), pp. 259-285.
Bunce, S. C., Noblett, K. L., McCloskey, M. S., & Coccaro, E. F. (2005). High prevalence of personality disorders among healthy volunteers for research: implications for control group bias. Journal of Psychiatric Research, 39(4), pp. 421-430.
Caligor, E., Kernberg, O. F., & Clarkin, J. F. (2007). Handbook of dynamic psychotherapy for higher level personality pathology. Washington, DC: American Psychiatric Publishing, Inc.
Chatham, P. (1989). Treatment of the borderline personality. Northvale, NJ: Jason Aronson.
Davidson, K., Norrie, J., Tyrer, P., Gumley, A., Tata, P., Murray, H., & Palmer, S, (2006). The effectiveness of cognitive behavior therapy for borderline personality disorder: Results from the borderline personality disorder study of cognitive therapy (BOSCOT) trial. Journal of Personality Disorders, 20(5), pp. 450-465.
Davidson, K., Livingstone, S., McArthur, K., Dickson, L., & Gumley, A. (2007). An integrative complexity analysis of cognitive behaviour therapy sessions for borderline personality disorder. Psychology and Psychotherapy: Theory, Research and Practice, 80(4), pp. 513-523.
Davidtz, J. (2008). Psychotherapy with difficult patients: Personal narratives about managing countertransference. Dissertation Abstracts International: Section B: The Sciences and Engineering, 68(7), 4818.
Dudeck, M., Spitzer, C., Stopsack, M., Freyberger, H.J., & Barnow, S. (2007). Forensic inpatient male sexual offenders: The impact of personality disorder and childhood sexual abuse. Journal of Forensic Psychiatry & Psychology, 18(4), pp. 494-506.
Dulit, R. A., Ryer, M. R., Leon, A. C., & Brodsky, B. S. (1994). Clinical correlates of self-mutilation in borderline personality disorder. American Journal of Psychiatry, 151(9), pp. 1305-1311.
Fonagy, P. (1998). An attachment theory approach to treatment of the difficult patient. Bulletin of the Menninger Clinic, 62(2), 147-169.
Fruzzetti, A. E. (2002). Dialectical behavior therapy for borderline personality and related disorders. In Kaslow, F. W., & Patterson, T. Comprehensive handbook of psychotherapy: Cognitive-behavioral approaches, Vol. 2. Hoboken, NJ: John Wiley & Sons Inc. pp. 215-240.
Furnham, A. (2007). Personality disorders and derailment at work: The paradoxical positive influence of pathology in the workplace. In: Langan-Fox, J., Cooper, C. L., & Klimoski, R. J. Research companion to the dysfunctional workplace: Management challenges and symptoms. Northampton, MA: Edward Elgar Publishing. pp. 22-39.
George, E. L., Miklowitz, D. J., Richards, J. A., Simoneau, T. L., & Taylor, D. O. (2003). The comorbidity of bipolar disorder and axis II personality disorders: prevalence and clinical correlates. Bipolar Disorders, 5(2), pp. 115-122.
Godt, K. (2002). Personality disorders and eating disorders: the prevalence of personality disorders in 176 female outpatients with eating disorders. European Eating Disorders Review, 10(2), pp. 102-109.
Grant, B. F., Hasin, D. S., Stinson, F. S., Dawson, D. A., Chou, S. P., Ruan, W. J., & Pickering, R. P. (2004). Prevalence, Correlates, and Disability of Personality Disorders in the United States: Results From the National Epidemiologic Survey on Alcohol and Related Conditions. Journal of Clinical Psychiatry, 65(7), pp. 948-958.
Hansen, B., Vogel, P. A., Stiles, T. C., & Götestam, K. G. (2007). Influence of co-morbid generalized anxiety disorder, panic disorder and personality disorders on the outcome of cognitive behavioural treatment of obsessive-compulsive disorder. Cognitive Behaviour Therapy, 36(3), pp. 145-155.
Hartman, D. (1999). Regarding the difficult patient.’. British Journal of Psychiatry, 175, 192.
Gutheil, T. G. (2004). Suicide, Suicide Litigation, and Borderline Personality Disorder. Journal of Personality Disorders, 18(3), 248-256.
Gutheil, T. G., & Alexander, V. (1992). Medicolegal issues between the borderline patient and the therapist. In D. Silver, M. Rosenbluth, D. Silver, M. Rosenbluth (Eds.) , Handbook of borderline disorders (pp. 389-413). Madison, CT, US: International Universities Press, Inc.
Hill, A., Habermann, N., Berner, W., & Briken, P. (2006). Psychiatric disorders in single and multiple sexual murderers. Psychopathology, 40(1), pp. 22-28.
Hobson, J., & Shine, J. (2008). Measurement of psychopathy in a UK prison population referred for long-term psychotherapy. British Journal of Criminology, 38(3), pp. 504-515.
Hoffman, P. D., Buteau, E. Hooley, J. M., Fruzzetti, A. E., & Bruce, M. L. (2003). Family members’ knowledge about borderline personality disorder: Correspondence with their levels of depression, burden, distress, and expressed emotion. Family Process, 42(4), pp. 469-478.
Høglend, P. (1993). Personality disorders and long-term outcome after brief dynamic psychotherapy. Journal Of Personality Disorders, 7(2), 168-181. doi:10.1521/pedi.1993.7.2.168
Johnson, D. M., Sheahan, T. C., & Chard, K. M. (2003). Personality Disorders, Coping Strategies, and Posttraumatic Stress Disorder in Women with Histories of Childhood Sexual Abuse. Journal of Child Sexual Abuse, 12(2), pp. 19-39.
Keown, P., Holloway, F., & Kuipers, E. (2002). The prevalence of personality disorders, psychotic disorders and affective disorders amongst the patients seen by a community mental health team in London. Social Psychiatry & Psychiatric Epidemiology, 37(5), p. 225.
Kernberg, (1985). Borderline Conditions and Pathological Narcissism. New York, NY: Rowman & Littlefield,
Kyrios, M., Nedeljkovic, M., Moulding, R., & Doron, G. (2007). Problems of employees with personality disorders: The exemplar of obsessive-compulsive personality disorder (OCPD). In Langan-Fox, J., Cooper, . L., & Klimoski, R. J. Research companion to the dysfunctional workplace: Management challenges and symptoms. Northampton, MA: Edward Elgar Publishing, pp. 40-57.
King, A. R. (2000). Relationships between CATI personality disorder variables and measures of academic performance. Personality and Individual Differences, 29(1), pp. 177-190.
Liebenberg, B. (1990). The unwanted and unwanting patient: Problems in group psychotherapy of the narcissistic patient. In B. E. Roth, W. N. Stone, H. D. Kibel, B. E. Roth, W. N. Stone, H. D. Kibel (Eds.) , The difficult patient in group: Group psychotherapy with borderline and narcissistic disorders (pp. 311-322). Madison, CT, US: International Universities Press, Inc.
Leichsenring, F., & Leibing, E. (2003). The Effectiveness of Psychodynamic Therapy and Cognitive Behavior Therapy in the Treatment of Personality Disorders: A Meta-Analysis. American Journal of Psychiatry, 160(7), pp. 1223-1232.
Lindsay, W., Hogue, T., Taylor, J., Mooney, P., Steptoe, L., Johnston, S., O’Brien, G., & Smith, A. (2006). Two studies on the prevalence and validity of personality disorder in three forensic intellectual disability samples. Journal of Forensic Psychiatry & Psychology, 17(3), pp. 485-506.
Linehan MM. (1993). Cognitive-Behavioral Treatment of BPD. New York, NY: Guilford Press.
Linehan, M. M., Comtois, K. A., Murray, A. M., Brown, M. Z., Gallop, R. J., Heard, H. L., Korslund, K. E., Tutek, D. A., Reynolds, S. K., & Lindenboim, N. (2006). Two-Year Randomized Controlled Trial and Follow-up of Dialectical Behavior Therapy vs Therapy by Experts for Suicidal Behaviors and Borderline Personality Disorder. Archives of General Psychiatry, 63(7), pp. 757-766.
López, D., Cuevas, P., Gómez, A., & Mendoza, J. (2007). Psicoterapia focalizada en la transferencia para el trastorno límite de la personalidad. Un estudio con pacientes femeninas. Salud Mental, 27(4), pp. 44-54.
Luk, J.M. (1991). Cognitive-behavioural group therapy for Hong kong Chinese adults with mental health problems. Australian and New Zealand Journal of Psychiatry, 25(4), pp. 524-534.
Lynch, T. R., & Horton, L. E. (2004). Personality Disorders. In Thomas, J. C. & Hersen, M. Psychopathology in the workplace: Recognition and adaptation. New York, NY: Brunner-Routledge, pp. 147-160.
Lynch, T. R., Trost, W. T., Salsman, N., & Linehan, M. M. (2007). Dialectical behavior therapy for borderline personality disorder. Annual Review of Clinical Psychology, 3, pp. 181-205.
Maina, G., Albert, U., Pessina, E., & Bogetto, F. (2007). Bipolar obsessive-compulsive disorder and personality disorders. Bipolar Disorders, 9(7), pp. 722-729.
Manelski, J. (2005). Distinguishing characteristics of victims of domestic violence: Personality disorders and communication skill deficits. Dissertation Abstracts International: Section B: The Sciences and Engineering, 65(8-B), p. 4294.
Markham, D. (2003). Attitudes towards patients with a diagnosis of ‘borderline personality disorder’: Social rejection and dangerousness. Journal of Mental Health, 12(6), pp. 595-612.
Massion, A. O., Dyck, I. R., Shea, M. T., Phillips, K. A., Warshaw, M. G., & Keller, M. B. (2002). Personality disorders and time to remission in generalized anxiety disorder, social phobia and panic disorder. Archives of General Psychiatry, 59(5), pp. 434-440.
Mavissakalian, M. R., Hamann, M. S., Haidar, S. A., & de Groot, C. M. (1995). Correlates of DSM-III personality disorder in generalized anxiety disorder. Journal of Anxiety Disorders, 9(2), pp. 103-115.
McDonald, J. J. (2002). Personality Disorders in Employment Litigation. Psychiatric Times. 19(4), pp. 1-5.
McGlashan, T. H., Grilo, C. M., Sanislow, C. A., Ralevski, E., Morey, L. C., Gunderson, J. G., Skodol, A. E., Shea, M. T., Zanarini, M. C., Bender, D., Stout, R. L., Yen, S., & Pagano, M. (2005). Two-year prevalence and stability of individual DSM-IV criteria for schizotypal, borderline, avoidant, and obsessive-compulsive personality disorders: Toward a hybrid model of axis II disorders. American Journal of Psychiatry, 162(5), pp. 883-889.
McLean, L. M., Gallop, R. (2003). Implications of childhood sexual abuse for adult borderline personality disorder and complex posttraumatic stress disorder. American Journal of Psychiatry, 160(2), pp. 369-371.
Millon, T., Blaneyu. P. H., & Davis R. (eds.) (1999). Oxford Textbook of Psychopathology. New York: Oxford University Press. pp. 510.
Moran, P., Jenkins, R., Tylee, A., Blizard, R., & Mann, A. (2000). The prevalence of personality disorder among UK primary care attenders. Acta Psychiatrica Scandinavica, 102(1), p. 52.
Moran, P., & Mann, A. (2002). The prevalence and 1-year outcome of cluster B personality disorders in primary care. Journal of Forensic Psychiatry, 13(3), pp. 527-537.
Morgenstern, J., & Miller, K. J. (1997). The comorbidity of alcoholism and personality disorders in a clinical population: Prevalence. Journal of Abnormal Psychology, 106(1), p. 74.
Narcisco, B. (2007). The relationships among trauma, self-concept, dissociation, Cluster B Personality Disorders and adult attachment style in incarcerated women. Dissertation Abstracts International: Section B: The Sciences and Engineering, 68(1-B), pp. 630.
Neeleman, A. J. F. (2007). The relevance of sexuality in the treatment of borderline personality disorder. Tijdschrift voor Psychiatrie, 49(4), pp. 233-240.
Paris, J. (2005). Understanding Self-mutilation in Borderline Personality Disorder. Harvard Review of Psychiatry, 13(3), pp. 179-185.
Pompili, M., Ruberto, A., Girardi, P., & Tatarelli, R. (2004). Suicidality in DSM IV Cluster B personality disorders: An overview. Ann ist Super Sanità, 40(4), pp. 475-483.
Quante, A., Röpke, S., Merkl, A., Anghelescu, I., & Lammers, C. (2008). Psychopharmakologische behandlung von und bei persönlichkeitsstörungen. Fortschritte der Neurologie, Psychiatrie, 76(3), 139-148. doi: 10.1055/s-2007-996179.
Roth, B. E., Stone, W. N., & Kibel, H. D. (1990). The difficult patient in group: Group psychotherapy with borderline and narcissistic disorders. , American Group Psychotherapy Association monograph series, Monograph; 6. Retrieved September 3, 2008, from http://search.ebscohost.com/login.aspx?direct=true&db=psyh&AN=1990-97241-000&site=ehost-live.
Rollnik, J. D., Schneider, U., Wedegaertner, F. Huber, T. J., & Emrich, H. M. (2001). Uncommon self-mutilation in a borderline personality disorder patient. Australian and New Zealand Journal of Psychiatry, 35(1), pp. 133-134.
Rothschild, B., & Rand, M. (2006). Help for the Helper: The Psychophysiology of Compassion Fatigue and Vicarious Trauma. NY, New York: W.W. Norton & Company.
Salsman, N. L., & Linehan, M. M. (2006). Dialectical-behavioral therapy for borderline personality disorder. Primary Psychiatry, 13(5), pp. 51-58.
Samuels J. F., Nestadt, G., Romanoski A. J., Folstein, M. F., & McHugh, P. R. (1994). DSM-III personality disorders in the community. American Journal of Psychiatry, 151, pp. 1055-1062.
Sansone, R. A., Levitt, J. L., & Sansone, L. A. (2005). The prevalence of personality disorders among those with eating disorders. Eating Disorders, 13(1), pp. 7-21.
Scheirs, J. G. M., & Bok, S. (2007). Psychological distress in caretakers or relatives of patients with borderline personality disorder. International Journal of Social Psychiatry, 53(3), pp. 195-203.
Sperry, L. (2006). Cognitive behavior therapy of DSM-IV-TR personality disorders: Highly effective interventions for the most common personality disorders (2nd ed.). New York, NY: Routledge/Taylor & Francis Group.
Thuo, J., Ndetei, D. M., Maru, H., & Kuria, M. (2008). The prevalence of personality disorders in a Kenyan inpatient sample. Journal of Personality Disorders, 22(2), pp. 217-220.
Volkan, K. (1994). Dancing among the Maenads: The psychology of compulsive drug use. New York, NY: Peter Lang.
Wilson, S. T., Stanley, B., Oquendo, M. A., Goldberg, P., Zalsman, G., & Mann, J. J. (2007). Comparing impulsiveness, hostility, and depression in borderline personality disorder and bipolar II disorder. Journal of Clinical Psychiatry, 68(10), pp. 1533-1539.
Zimmerman, M., Rothschild, L., & Chelminski, I. (2005). The Prevalence of DSM-IV Personality Disorders in Psychiatric Outpatients. American Journal of Psychiatry, 162(10), pp.1911-1918.
—————
1. Interestingly enough it seems that being a victim of domestic violence rather than the perpetrator is not related to having a personality disorder. In fact, some personality disorders may be inversely related to being the victim of domestic violence (Manelski, 2005).
2. DBT combines Cognitive Behavior Therapy with mindfulness techniques from Buddhist psychology.
 |
| Leopoldo Fregoli |
This delusion is named after the Italian actor Leopoldo Fregoli, who often changed appearances and identities during his performances. This type of delusion occurs when a person believes that a number of different people are actually one person who has the ability to change their appearance. The different people are usually familiar and are often considered to be hostile or persecutory to the Fregoli sufferer. This delusion is often thought of as a variant of Capgras Syndrome and it seems the underlying neuropathology is similar, usually involving lesions to the right hemisphere of the brain. It has been difficult however, to clearly trace the delusional misidentification directly to the organic pathology since the syndrome is so often comorbid with psychotic disorders (Mojtabai, 1994; Novakovic, Aje, & Sher, 2010).
One research study has reported that Capgras, Fregoli, and psychotic syndromes can be distinguished from one another by observing facial recognition reaction times. Patients suffering from delusional misidentification disorders had longer took longer to perform facial recognition tasks than psychotic patients, with Fregoli patients taking longer than Capgras patients. This may indicate differences in underlying pathology among psychotic, Capgras and Fregoli syndromes (Walther et al., 2010).
In addition to psychoses, Fregoli syndrome has been associated with a number of other disorders. Bruggemann and Garlip report a case of erotomania combined with Fregoli delusion in a 24 year old woman. This woman believed a colleague who was the target of her erotomania, appeared as other people. While they did not find any overt pathology they did note EEG differences in the right temporal lobe. This woman, as is typical for people with Fregoli syndrome, also suffered from psychotic symptoms such as imagining she had become pregnant by her colleague and that she was his fiancée. She was treated via psychotherapy and neuroleptic medication, which lessened her symptoms. When the patient stopped taking her medication her psychotic symptoms returned. The authors conclude that the Fregoli syndrome was secondary to paranoid schizophrenia (Brüggemann & Garlipp, 2007).
Melca et. al. (2012) describe two patients with delusional misidentification disorders (Vapgras and Fregoli syndromes) who also suffered from treatment resistant obsessive compulsive disorder (OCD). One of the two patients also was diagnosed with paranoid personality disorder while the other with pervasive developmental disorder. Both patients in the study exhibited varying amounts of insight related to their OCD. The authors speculate that there may be a relationship between OCD and delusional misidentification disorders (DMS).
Fregoli syndrome has also been associated with violent behavior. Delavenne & Garcia (2011) report on a case of a paranoid schizophrenic woman who was convinced that a boyfriend was able to appear as other people so he could follow her. This patient had an episode of violent behavior associated with her Fregoli delusion. She had topped taking her anti-psychotic medication 6 months prior to her violent outburst. Facial recognition tests and a CT scan of her brain revealed no abnormalities. Even though she was put back on anti-psychotic medication, her delusions returned after 10 days.
Fregoli syndrome has also been associated with bipolar schizoaffective disorder and Hashimoto’s thyroiditis (Ceylan et al., 2010).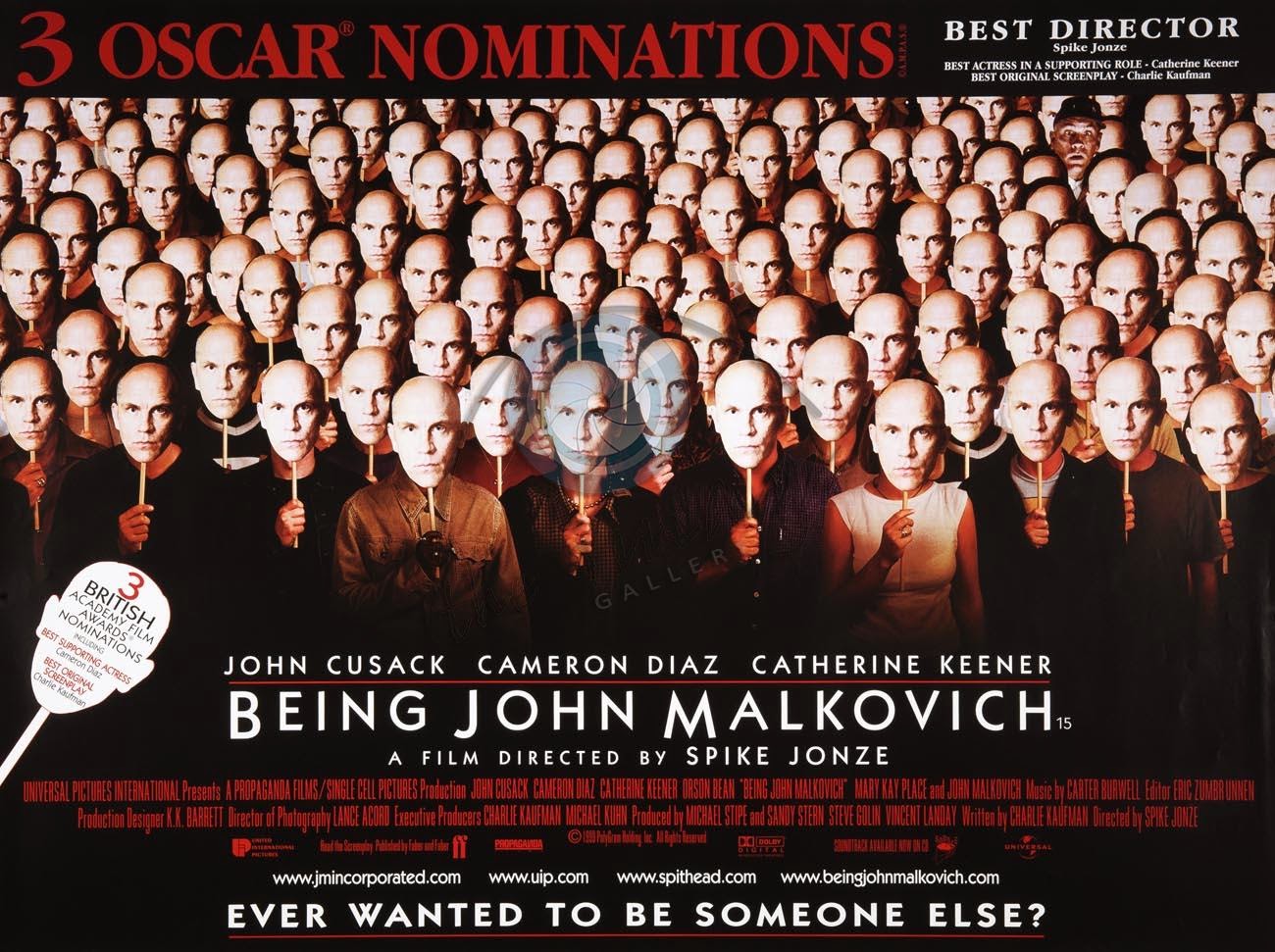
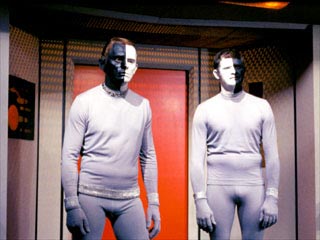
Delusional Misidentification Syndrome in the form of Fregoli Delusion has also made appearances in popular culture. One of the best examples of this is a variant of Fregoli Delusion which is central to the film Being John Malkovich (Jonze, 1999). In this film there is a tunnel in a strange half floor of an office building. Travel through this tunnel allows people to experience ‘being’ the actor John Malkovich for a short time. Later in the film, John Malkovich himself discovers the existence of the tunnel and goes through it. When he emerges everyone else is a version of Malkovich, with his face and everything they say coming out as the word ‘Malkovich’.
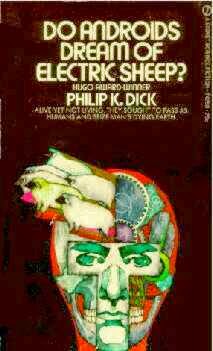
 Science fiction has been an especially fruitful ground for the emergence of modern stories related to imposters masquerading as humans. This can be seen most readily in stories about robots or androids. In many cases these stories revolve around the ‘imposters’ wanting to become human, or being indistinguishable from humans, as in the Phillip K. Dick story Do Androids Dream of Electric Sheep? (1968/1996), which was made into the movie Blade Runner (Scott, 1982), or the Isaac Asimov Robot series (1982) which has had a number of film adaptations including most recently the film I Robot (Proyas, 2004). In these modern portrayals humans are generally anxious about the imposter status of the robots and androids as well as being paranoid about their intentions. It is possible that the popularity of the imposters among us theme relates to a subconscious fear of misidentification in general.
Science fiction has been an especially fruitful ground for the emergence of modern stories related to imposters masquerading as humans. This can be seen most readily in stories about robots or androids. In many cases these stories revolve around the ‘imposters’ wanting to become human, or being indistinguishable from humans, as in the Phillip K. Dick story Do Androids Dream of Electric Sheep? (1968/1996), which was made into the movie Blade Runner (Scott, 1982), or the Isaac Asimov Robot series (1982) which has had a number of film adaptations including most recently the film I Robot (Proyas, 2004). In these modern portrayals humans are generally anxious about the imposter status of the robots and androids as well as being paranoid about their intentions. It is possible that the popularity of the imposters among us theme relates to a subconscious fear of misidentification in general.
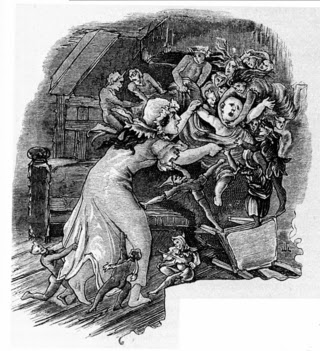
 An older instance of DMS can be found primarily in the British Isles. In times past British or Celtic babies were thought to be kidnapped by fairies and replaced by identical looking children. The replacement children, called changelings, were often sickly and exhibited abnormal behavior.
An older instance of DMS can be found primarily in the British Isles. In times past British or Celtic babies were thought to be kidnapped by fairies and replaced by identical looking children. The replacement children, called changelings, were often sickly and exhibited abnormal behavior.
Evans (2000) describes the Irish belief in changelings that is typical of the British Isles;
Mothers and babies were thought to be especially liable to be abducted by the fairies, and protective charms were hidden in a baby’s dress or placed in the cradle. When children were taken to be baptized, too, special preparations were made and precautions taken, for example, a County Antrim clergyman reported that his parishioners would place a piece of bread and cheese in the child’s clothing.
The old custom of dressing boys in girls’ clothes, in long frocks, until they were ten or eleven years of age has been explained as a means of deceiving the fairies, who were always on the lookout for healthy young boys whom they could replace by feeble “changelings.” For the same reason it is unwise to praise a child without adding a saving “God bless him,” and young boys are still half jocularly referred to as “rogues and Tories.” The belief in “changelings” may have arisen as an explanation of the high mortality rate among baby boys as compared with girls. (p. 289)
Indeed, changeling legends may be related to high infant mortality rates in general. When an infant becomes sick and dies for no apparent reason, the human mind will seek an explanation for such a tragic event. If no logical reason can be found the human mind invents a reason that can provide meaning to the tragedy and lessen its sting. There is always a chance the original child can be returned by the fairies, or the thought the original child is being raised by the fairies and has been given special powers can be of comfort to the grieving parents.
The changeling legends have much in common with the belief in the ‘evil eye’ that has its origins in the Mediterranean regions. In this legend it is especially important to ward off the evil eye from infants who are susceptible to its negative influence. I hope to write more extensively about belief in the evil eye, as it has some unique and interesting features.
References
Asimov, I. (1982). The Complete Robot (1st ed.). Doubleday.
Brüggemann, B. R., & Garlipp, P. (2007). A special coincidence of erotomania and fregoli syndrome. Psychopathology, 40(6). http://doi.org/10.1159/000108127
Ceylan, M. F., Bulut, M., Virit, O., Selek, S., Bülbül, F., & Sava?, H. A. (2010). Hashimato tiroiditi olan eri?kin bipolar bozukluk hastasinda capgras ve fregoli sendromu birlikteli?i. Yeni Symposium: Psikiyatri, Nöroloji ve Davrani? Bilimleri Dergisi, 48(1), 69–71.
Delavenne, H., & Garcia, F. D. (2011). Fregoli syndrome associated with violent behavior. Jornal Brasileiro de Psiquiatria, 60(1), 71–72. http://doi.org/10.1590/S0047-20852011000100014
Dick, P. K. (1996). Do Androids Dream of Electric Sheep?. Del Rey.
Evans, E. E. (2000). Irish Folk Ways. Courier Dover Publications.
Jonze, S. (1999). Being John Malkovich. Comedy, Drama, Fantasy.
Melca, I., Rodrigues, C., Serra-Pinheiro, M., Pantelis, C., Velakoulis, D., Mendlowicz, M., & Fontenelle, L. (2012). Delusional Misidentification Syndromes in Obsessive–Compulsive Disorder. Psychiatric Quarterly, 1–7. http://doi.org/10.1007/s11126-012-9237-z
Mojtabai, R. (1994). Fregoli syndrome. Australian and New Zealand Journal of Psychiatry, 28(3), 458–462. http://doi.org/10.3109/00048679409075874
Novakovic, V., Aje, O., & Sher, L. (2010). A patient with the Fregoli syndrome: A case report and discussion of the relevant literature. International Journal on Disability and Human Development, 9(1), 81–83. http://doi.org/10.1515/IJDHD.2010.012
Proyas, A. (2004). I, Robot. Action, Mystery, Sci-Fi, Thriller.
Scott, R. (1982). Blade Runner. Drama, Sci-Fi, Thriller.
Walther, S., Federspiel, A., Horn, H., Wirth, M., Bianchi, P., Strik, W., & Müller, T. J. (2010). Performance during face processing differentiates schizophrenia patients with delusional misidentifications. Psychopathology, 43(2), 127–136. http://doi.org/10.1159/000277002
In order to understand many bizarre behaviors it is important to have some understanding of personality disorders. These are the most common of the serious mental illness and are seemingly related to many bizarre behaviors seen around the world. People suffering from these disorders tend to exhibit emotional patterns and behaviors that seem troubling to the majority of people and are not necessarily explicable by immediate environmental stimuli. Nevertheless many clinicians are unfamiliar with the most recent research on these disorders and the latest approaches to treatment. This article review the current diagnostic conceptualization of personality disorders, their clinical treatment, and their relationship to cultural characteristics and culture-specific disorders. Below I present an overview of the main diagnostic categories related to personality disorders. This is just a quick skim of the surface and I refer to the reader to the DSM-V (American Psychiatric Association, 2013) for greater detail.
Diagnosis of Personality Disorders
In the creation of the new DSM-V there was some debate about what to do with the diagnostic category for personality disorders. In the end the creators of the DSM-decided to holdover the different types of personality disorders from the DSM-IV but to remove these disorders from a separate axis. The DSM-V also keeps the same cluster structure as in the DSM-IV. The DSM-V: Diagnostic and Statistical Manual of Mental Disorders (American Psychiatric Association, 2013) defines the following criteria for the diagnosis of a personality disorder:
A. An enduring pattern of inner experience and behavior that deviates markedly from the expectations of the individual’s culture. This pattern is manifested in two (or more) of the following areas:
- 1. Cognition (i.e., ways of perceiving and interpreting self, other people, and events).
- 2. Affectivity (i.e., the range, intensity, lability, and appropriateness of emotional response).
- 3. Interpersonal functioning.
- 4. Impulse control.
B. The enduring pattern is inflexible and pervasive across a broad range of personal and social situations.
C. The enduring pattern leads to clinically significant distress or impairment in social, occupational, or other important areas of functioning.
D. The pattern is stable and cf long duration, and Its onset can be traced back at least to adolescence or early adulthood.
E. The enduring pattern is not better explained as a manifestation or consequence of another mental disorder.
F. The enduring pattern is not attributable to the physiological effects of a substance (e.g.,a drug of abuse, a medication) or another medical condition (e.g., head trauma). (p. 646-647)
There are ten types of personality disorders recognized in the DSM V: Schizotypal, Paranoid, Schizoid, Antisocial, Borderline, Obsessive-Compulsive, Dependent, Avoidant, Narcissistic, and Histrionic. Briefly, these can be understood to have the following characteristics:
Antisocial Personality Disorder: People suffering from this disorder are characterized as having a disregard for moral or legal standards of their culture. They have trouble getting along with others and/or following the rules of society. They used to be called psychopaths or sociopaths.
Avoidant Personality Disorder: People suffering from this disorder have heightened social inhibitions combined with feelings of inadequacy. These people generally are extremely sensitive to criticism.
Borderline Personality Disorder: People with this disorder lack a stable identity. They may be emotionally labile and have unusually intense, yet unstable relationships with others. Persons suffering from this disorder also have marked impulsivity, and often are dissociated from their emotions.
Dependent Personality Disorder: People with this disorder have an extreme need of other people. They have trouble doing anything on their own and are often unable to make decisions or be independent in any aspects of their lives. They have an intense fear of separation, which may manifest itself in extremely submissive and conciliating behavior. People with this disorder lack self-confidence and self-esteem.
Histrionic Personality Disorder: People with this disorder are overly dramatic with highly exaggerated and/or inappropriate emotional displays. They manifest sudden and rapidly shifting expression of emotions that often seem fake or shallow.
Narcissistic Personality Disorder: People with this disorder see themselves as most important person in the universe, emanating grandiosity and omnipotence. They also lack empathy toward others while at the same time needing other people’s admiration and attention. This lack of empathy makes it difficult for them to understand other’s points of view making them intolerant and hypersensitive to criticism.
Obsessive-Compulsive Personality Disorder: People suffering from this disorder tend to be perfectionists and are inflexible. The disorder manifests as repetitive patterns of thought and/or behavior that the person feels are out of his or her control.
Paranoid Personality Disorder: This disorder is characterized by an extreme distrust of others. This distrust can become extreme to the point where a person’s paranoid beliefs (i.e. that others are exploiting, harming, or trying to deceive) are thought disordered, containing their own set of internal logic unrelated to consensus reality. People suffering from this disorder often believe that they have been betrayed and that there is hidden significance in the behavior of others. People with this disorder are often unforgiving and hold grudges.
Schizoid Personality Disorder: Those suffering from this disorder have a very limited range of emotional expression and experience. They present as being very ‘flat’, withdrawn and uninterested in social relationships.
Schizotypal Personality Disorder: This disorder is similar to schizophrenia except that it does not include frankly psychotic features such as hallucinations. Like schizophrenia however, it does include disordered thoughts, magical beliefs and thought patterns1. People with this disorder may appear or behave in an eccentric or disordered fashion as well as evincing belief in things that make no logical sense.
Also included in the DSM-V are two further categories, which are self-explanatory:
Personality change due to another medical condition is a persistent personality disturbance that is judged to be due to the direct physiological effects of a medical condition (e.g., frontal lobe lesion).
Other specified personality disorder and unspecified personality disorder is a category provided for two situations: 1) the individual’s personality pattern meets the general criteria for a personality disorder, and traits of several different personality disorders are present, but the criteria for any specific personality disorder are not met; or 2) the individual’s personality pattern meets the general criteria for a personality disorder, but the individual is considered to have a personality disorder that is not included in the DSM-5 classification (e.g., passive-aggressive personality disorder). (American Psychiatric Association, 2013, p. 645)
The DSM-V (American Psychiatric Association , 2013), organizes personality disorders into three groups or clusters, with three or four disorders per group:
Cluster A – Eccentric Personality Disorders: Paranoid, Schizoid, Schizotypal: People suffering from these disorders often appear odd or peculiar and begin to demonstrate these aspects of the disorder by early adulthood and in various contexts.
Cluster B – Dramatic Personality Disorders: Antisocial, Borderline, Histrionic, and Narcissistic: People suffering from these disorders have intense, unstable emotions, distorted self-perception, and are often behave in impulsive ways.
Cluster C – Anxious Personality Disorders: Avoidant, Dependent, Obsessive-Compulsive: People suffering from these disorders are often anxious and fearful. They begin to demonstrate these aspects of the disorder by early adulthood and in various contexts.
The DSM-V also notes that it is often difficult to separate the diagnoses of schizophrenia and personality disorder. The reported prevalence of personality disorders among people suffering from schizophrenia varies tremendously – from 4.5% to 100%. It has been suggested that type of care, country, study type, and diagnostic tools all bias prevalence rates. (Newton-Howes, et. al. 2008). Structural magnetic resonance imaging and computer tomography studies suggest that schizotypal personality disorder may in fact be a milder form of schizophrenia. Normal volume and perhaps functioning of the medial temporal lobes in those suffering from schizotypal personality disorder may explain why schizophrenics (who have abnormal medial temporal lobes) experience more severe psychotic symptoms Dickey, McCarley, &; Shenton, 2002).
Next Part II: Co-morbidity & Prevalence
References
American Psychiatric Association. (2013). Diagnostic and Statistical Manual of Mental Disorders, 5th edition. Washington, DC: American Psychiatric Association.
Dickey, C. C., McCarley, R. W., & Shenton, M. E., (2002). The brain in schizotypal personality disorder” A review of structural MRI and CT findings. Harvard Review of Psychiatry, 10(1), pp. 1-15.
Newton-Howes G, Tyrer P, North B, Yang M. (2008). The prevalence of personality disorder in schizophrenia and psychotic disorders: systematic review of rates and explanatory modelling. Preview Psychological Medicine, 38(8), pp. 1075-1082.
Verheul, R., Bartak, A., & Widiger, T. (2007). Prevalence and construct validity of personality disorder not otherwise specified (pdnos). Journal of Personality Disorders, 21(4), pp. 359-370.
Children conceived by a sperm donor are worried that they will have an intimate relationship with an unknown, blood relative.